Understanding the Difference Between Meningioma and Glioma
When it comes to brain tumors, two common types that often cause concern are meningioma and glioma. While both are serious conditions that affect the brain, they have distinct characteristics and require different approaches for diagnosis and treatment. In this article, we’ll delve into the details of these two conditions, highlighting their differences, similarities, and the impact they can have on patients’ lives.
Introduction
Brain tumors, regardless of their type, can be life-altering and require prompt medical attention. Understanding the specific characteristics of different brain tumors is crucial for accurate diagnosis and effective treatment.
2. Understanding Meningioma
Definition and Characteristics
Meningioma is a type of brain tumor that originates in the meninges, which are the protective membranes covering the brain and spinal cord. These tumors are often benign (non-cancerous) and grow slowly over time.
Causes and Risk Factors
The exact causes of meningioma are not yet fully understood. However, certain risk factors, such as age, gender, and exposure to ionizing radiation, have been associated with an increased likelihood of developing this type of tumor.
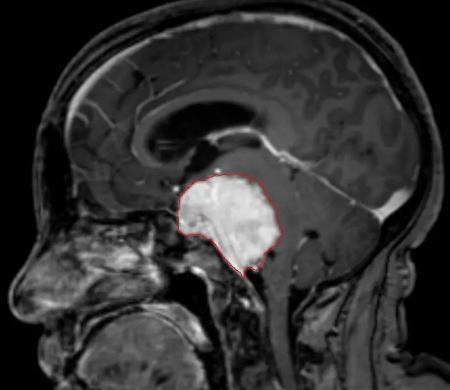
Symptoms and Diagnosis
The symptoms of meningioma can vary depending on the size and location of the tumor. Common symptoms include headaches, seizures, changes in vision or hearing, and cognitive impairments. Diagnosis typically involves a combination of imaging tests, such as MRI or CT scans, and a biopsy to confirm the presence of a meningioma.
Treatment Options
Treatment options for meningioma depend on factors like tumor size, location, and overall health of the patient. These may include watchful waiting, surgery, radiation therapy, or targeted drug therapy. The goal is to remove or control the tumor while preserving brain function.
Understanding Glioma
Definition and Types
Gliomas are a group of tumors that develop from glial cells, which are supportive cells in the brain. They can be further categorized into different types based on the specific glial cell they originate from, such as astrocytoma, oligodendroglioma, and ependymoma.
Causes and Risk Factors
The exact causes of gliomas are not fully understood. However, certain genetic mutations and environmental factors, including exposure to certain chemicals or radiation, have been linked to an increased risk of developing these tumors.
Symptoms and Diagnosis
The symptoms of glioma can vary depending on the tumor’s location and size. Common symptoms include headaches, seizures, memory loss, changes in mood or behavior, and neurological deficits. Diagnosis involves a combination of imaging tests, such as MRI or PET scans, and a biopsy to confirm the presence of a glioma.
Treatment Options
Treatment options for glioma depend on factors like tumor type, grade, Certainly! I apologize for the interruption. Please find the continuation of the article below.
Key Differences between Meningioma and Glioma
While both meningioma and glioma are brain tumors, they differ in several key aspects, including:
Location and Origin
Meningiomas primarily develop in the meninges, the protective membranes surrounding the brain and spinal cord. Gliomas, on the other hand, originate from glial cells within the brain itself.
Cellular Characteristics
Meningiomas are typically composed of cells resembling the meninges, while gliomas consist of abnormal glial cells. This difference in cellular composition contributes to variations in tumor behavior and response to treatment.
Growth Rate and Invasiveness
Meningiomas tend to grow slowly and often have well-defined borders, making them more amenable to surgical removal. Gliomas, however, can exhibit aggressive growth patterns, infiltrating surrounding brain tissue and making complete surgical resection more challenging.
Symptoms and Prognosis
The symptoms of meningioma and glioma can overlap, including headaches, seizures, and neurological deficits. However, specific symptoms may vary depending on the location of the tumor within the brain. Prognosis also differs, with meningiomas generally having a more favorable outcome compared to gliomas, which can be more challenging to treat successfully.
Similarities between Meningioma and Glioma
While there are significant differences between meningiomas and gliomas, it’s important to note some similarities as well. Both types of tumors can cause symptoms related to increased intracranial pressure, such as headaches and visual disturbances. Additionally, both require a multidisciplinary approach to diagnosis and treatment, involving neurosurgeons, neurologists, oncologists, and radiation oncologists.
Conclusion
In conclusion, understanding the difference between meningioma and glioma is crucial for accurate diagnosis and effective treatment planning. Meningiomas and gliomas have distinct origins, cellular characteristics, growth patterns, and prognoses. Identifying these differences enables healthcare professionals to provide tailored care and support to patients facing these challenging conditions.
FAQs
Q1. Can meningiomas turn into gliomas?
A1. No, meningiomas and gliomas are distinct tumor types with different cellular origins. Meningiomas do not transform into gliomas.
Q2. Are all meningiomas benign?
A2. While the majority of meningiomas are benign, some can be malignant (cancerous). Malignant meningiomas are less common but require more aggressive treatment.
Q3. Can gliomas be cured?
A3. Complete cure of gliomas is challenging due to their invasive nature. Treatment aims to control the tumor growth, manage symptoms, and prolong survival.
Q4. Are there any non-surgical treatment options for meningioma and glioma?
A4. Yes, non-surgical treatment options for both meningioma and glioma include radiation therapy and targeted drug therapy, depending on the specific characteristics of the tumor.
Q5. What are the long-term effects of meningioma and glioma treatment?
A5. The long-term effects of treatment can vary depending on factors such as tumor location, treatment modality, and individual patient factors. Some common long-term effects may include cognitive changes, hormonal imbalances, and neurological deficits.
Read More: India Royale Before Surgery




